The decision to sit or stand at work will affect millions of people and cost hundreds of millions of dollars every year. The ability to measure postural muscle strength in the workplace will allow us to choose postures that will not only minimize long-term health risks, but also make upright postures easier to sustain and minimize orthopedic problems.
Sitting vs. Standing
Standing may not solve the original trouble from sitting badly, and it may cause other health problems. People are reluctant to move from relaxed sitting to standing1-3, and standing may not have the uniform, positive effect on health that we expect over the long term 4-5. In short, standing may cause more trouble than it solves. If reclined sitting does not have enough muscle activity, and standing requires too much effort, what amount of muscle activity is just right? Ultimately, finding the middle ground between too little and too much postural effort at work may be more important than we previously thought.
Steady activity in the postural muscles is extremely important for long-term health. Without a way to measure how those muscles work, an ergonomics consultant can only guess about when to sit or stand.
Figure 1. ANSI-HFES Work Postures:
This diagram shows the generally accepted and recommended postures for work, and each one presumes neutral spine position. The images are shown in order of increasing muscle activity required to sustain the posture. The Reclined Sitting posture at the far left is the most relaxed and requires the least effort. The Standing posture at the right requires the most effort. The two middle postures (Upright Sitting, second, and Declined Sitting, third) have an upright torso position, but they differ in the height of the hip (or the seat pan) relative to the knee. Those postures also differ in the relative muscle effort needed to sustain the upright posture.
We need to find strong posture!
Our last blog commented on spine position, specifically how to know when people sit badly6-9. Unless we look closely, the difference between the best and the worst sitting spine posture may not easily be seen. Good posture is more evident when there is some movement of the postural muscles at the low back. When the movement is easily available, the posture can be sustained more easily. The key is to find how to sustain the strong functional position without working too hard.
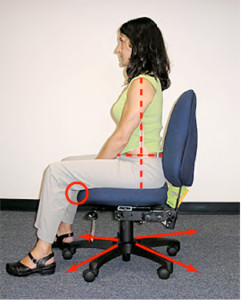
Photographs 1 and 2. Reclined and Perched Seated Postures. The top image shows the ‘recommended’ reclined sitting posture with good spine posture and low disc pressure compared to standing. The bottom image shows the same chair adjustment, but the body is upright and forward on the chair to get good spine posture for work that needs the torso “forward.” Even though the spine is in good position, there is not much support from the chair. Unless the chair and workstation are adjusted to support the strong posture shown in Photograph 2., the body will eventually slump when support is needed to relax.
The Postural Muscles
The postural muscles are the deep muscles in the legs and torso that hold the body upright. The measuring the intensity of that muscle work is similar to checking the engine temperature for your body. Much like there is an optimal temperature range for a motor, the body works best when there is a mid-range of muscle activity. Steady, regular activity of the postural muscles stimulates an enzyme called lipoprotein lipase, or LPL, that controls blood sugar and cholesterol metabolism. When the body is relaxed, the motor slows down, and the LPL enzyme activity almost completely stops10,11. Sustained postures without LPL activity cause increased blood sugar levels with more “bad” cholesterol levels and higher blood pressure12,13. When the postural muscles are steadily engaged to hold the body upright, the LPL enzyme activity returns, and the body recovers to work normally14.
What if we had a field measure to show when bodies can sustain their best posture?
We know what happens to the body when postural muscles are too relaxed over the long term. Using the temperature analogy, working the motor too hard creates another set of problems. Increasing the amount of effort to stand or walk at work has been shown to increase the risk of heart disease and varicose veins when compared to people who do not stand and walk as much15,16. Spine posture is an important measure for musculoskeletal problems, but good posture must also be easily sustained. Currently, there is no field measure to show when bodies can sustain their best working posture.
There are very sophisticated ways to measure how hard a muscle works, but those studies are usually done in a laboratory with precisely calibrated equipment. Using special equipment to measure everyone may not be effective. Average values have been calculated for the body effort to sustain different postures, but because of the wide range of physical ability between different people, and the differences from individual posture, those averages are not particularly useful (See MET’s note below).
Chair Height Affects Postural Muscle Strength
Small differences in chair height show measurable differences in leg strength. When we consistently challenge the leg and postural muscles at different chair heights, it is clear one height works best. Those small differences in chair heights can be measured in three different ways. First, the person in the chair can feel how easily the chair moves to a regular movement pattern (subjective report). Second, an observer can see the chair accelerate and decelerate more quickly, and the subject’s body appears to move easier at the best height (trained observer). Third, an accelerometer can measure the average acceleration and deceleration values to show when the forces at the best height are greatest (objective measure). The average leg torque values are calculated with an equation where the recorded force is equal to the body mass (which presumably remains constant during the test) times the acceleration value, or F=MA. There is a precise chair height where the leg and torso muscles are strongest, and that position is where the body can most easily balance and sustain the strongest position.
Photograph 3. Image of the chair movement challenge to determine best postural muscle strength. The subject uses a chair with a level seat pan and sufficient clearance for the legs. Holding the torso upright, the subject moves the chair in a regular pattern at several heights until the easiest height is determined.
If the chair is too high, the postural muscle in the legs and torso does not have sufficient mechanical advantage to easily move and support the body. If the chair is too low, the muscle at the hip and pelvis moves the torso back into reclined postures. The strongest position for the legs and postural muscle is the chair height where the body can most easily move the chair in each direction with the torso upright. That position allows balanced sitting for the pelvis at the precise height where the body can move in every direction, and most easily sustain upright posture.
Statistical Analysis
A study for this method was done ten years ago, letting the subject choose the best height. That data showed remarkably consistent results for each person with a very small height deviation (within one-quarter of an inch). Interestingly, although the subjects blindly picked their same height almost exactly each time in six trials, the angle of the thigh was different between subjects. It seems reasonable to conclude that postural muscle strength may be the better criteria to choose working postures, rather than using arbitrary hip angles, which will not consistently represent the best strength between subjects.
ActivSeating™ Methodology for Best Functional Posture
Using the priority to find the best functional posture strength for upright sitting rather than the contemporary method of reclined seated postures15 has been a practice tested for more than fifteen years. The approach does not need sophisticated training or equipment, although research measures can be correlated objectively with accelerometer data (HipTorque™). Testing the chair height is done in a few minutes with standard office seating, and workstation measures are derived from that position.
The basic principles of this ActivSeating™ approach are three:
- Select a chair height with the postural muscles most easily engaged
- Support the feet on the floor
- Put the forearms fully on the work surface
Aside from moving the surface height of the desk to meet the client stature, few new products are needed. When the principles of spinal posture and spinal muscle engagement are integrated with the clinical evidence from successful ergonomic strategies for the keyboard and point device17-24, the results address not only the immediate response from musculoskeletal symptoms, but they address the risk factors for the physiological risks for diabetes, obesity and heart disease.
Client Feedback on ActivSeating™ Methodology
Most of my clients are those who report persistent musculoskeletal symptoms after having had standard office ergonomics instruction and intervention with the customary guidelines: a reclined chair with a keyboard tray/arm, ergonomic keyboard, mouse, telephone headset and copyholder. A recent retrospective, single survey email questionnaire was sent to 1,000 of my clients in a large bank that were seen once in five years. These people had a wide range of symptoms and severity of injury, and at the time of the initial visit, most presented with a treatable injury. The survey response was slightly more than 15 percent (157 people), and the survey results from the single intervention were remarkable: 94% reported greater productivity, 92% reported fewer symptoms, and less than 2% reported symptoms that still affected their work. Fortunately, nobody reported that they were worse from the long-term effects of the program.
These consultations were provided in a community of predominantly conventional, modular panel-supported workstations, using conventional (Herman-Miller) ergonomic chairs. Sit-stand workstations constituted less than two percent (2.0%) of the observed furniture, and were not considered for recommendation unless there was a physician’s order.
Graphs of the survey responses for productivity and discomfort follow:
Did the ergonomics consultation improve your work productivity? (148 respondents)
| Very effective improvement | 62% (91 people) |
| Moderate improvement | 33% (49 people) |
| Neutral improvement | 5% (8 people) |
| Reduced productivity | 0% (0 people) |
[/custom_table]
Was the consultation effective to reduce your work symptoms? (147 respondents)
| Very effective | 58% (86 people) |
| Moderate | 34% (50 people) |
| Neutral | 7% (10 people) |
| Not effective | 0% (0 people) |
[/custom_table]
Do symptoms still currently affect your work? (150 respondents)
| Not at all | 59% (89 people) |
| Somewhat affect work | 34% (51 people) |
| Moderately affect work | 5% (7 people) |
| Definitely affect work | 2% (3 people) |
[/custom_table]
Note on MET’s: Average values for the amount of effort needed to sustain many different postures and activities can be estimated and predicted. Because there is a so much variation between different bodies’ size, stature and metabolism, even direct measurement for someone in one activity or posture may only vaguely predict the amount of work required for anyone else to do exactly the same thing. As an example, one measure of effort is called a Metabolic Equivalent Time, or MET, and that measure is based on the body size, mass and surface area, and a number is then calculated for how efficiently the body can do any specific task, like sitting, standing, walking, running, etc. The amount of effort needed to sustain several work postures has been calculated: reclining back in the chair requires from 1.0 to 1.5 MET’s—that posture is considered sedentary with the least postural muscle activity and the greatest health risk (Owen). Standing, which is considered a non-sedentary posture, has an estimated work range between 2.5 and 2.9 MET’s, but standing and walking also have associated health risks. Because there is so much variation in posture, and the variation for postural muscle engagement may be more directly representative of health risk, the author believes that postures selected for their value of postural muscle engagement may be more pertinent.
John Fitzsimmons is a Certified Industrial Ergonomist and a Physical Therapist skilled with treating musculoskeletal injuries. He is the principal consultant for Ergonomics First, Inc.
References:
- Robertson M, Ciriello M, Garabet M, 2013. Office ergonomics training and a sit-stand workstation: effects on musculoskeletal and visual symptoms and performance of office workers. Applied Ergonomics (44) 73-85.
- Straker, L, et al., 2013. Sit-stand desks in call centres: Associations of use and ergonomics awareness with sedentary behavior. Applied Ergonomics (44) 517-522.
- Wilks S, Mortimer M, Nylen P. 2006. The introduction of sit-stand tables: aspects of attitudes, compliance and satisfaction. Applied Ergonomics (37) 359-365.
- Gilson N, et al., Does the use of standing ‘hot’ desks change sedentary work time in an open plan office? Preventive Medicine (54) 65–67
- Karakolis T, Callaghan J. The impact of sit-stand office workstations on worker discomfort and productivity: A review. Applied Ergonomics (45) 799-806.
- Fitzsimmons J. 2014. Improving field observations of spinal posture in sitting. Ergonomics in Design (22) 23-26
- Pynt J, Higgs J, Martin M. 2001. Seeking the optimal posture of the seated spine. Physiotherapy Theory and Practice (17) 5-21, Taylor & Francis
- Dunk N, Kedgley A, Jenkyn T, Callagahan J. 2009. Evidence of a pelvis-driven flexion pattern: are the joints of the lower spine fully flexed in seated postures? Clinical Biomechanics (24) 164-168
- Panjabi M, 1992. The stabilizing system of the spine. Part II. Neutral zone and instability hypotheses. J Spinal Disord (5) 390-397.
- Bey L, Hamilton M. 2003. Suppression of skeletal muscle lipoprotein lipase activity during physical inactivity: a molecular reason to maintain daily low-intensity activity J Physiol (551) 673-682
- Hamilton M, Hamilton D, Zderic T. 2004. Exercise physiology versus inactivity physiology: an essential concept for understanding lipoprotein lipase regulation. Exerc Sport Sci Rev (32) 161-166
- Healy G, et. al., 2008. Television time and continuous metabolic risk in physically active adults. Med Sci Sports Exerc. (40) 639-45
- Owen N, Healy G, Matthews C, Dunstan D, 2010. Too much sitting: the population-health science of sedentary behavior. Exerc Sport Sci Rev. (38) 105-113
- Warren T, et.al, 2010. Sedentary behaviors increase risk of cardiovascular disease mortality in men Med Sci Sports Exerc (42) 879-885
- Krause, N, et al., 2007. Occupational activity, energy expenditure and 11-year progression of carotid atherosclerosis. Scandinavian Journal of Work and Environmental Health (33) 405-424
- Tüchsen, F, Hannerz, H, Burr H, and Krause N. 2005. Prolonged standing at work and hospitalization due to varicose veins: a 12-year prospective study of the Danish population. Occupational Environmental Medicine (62) 847-850.
- Dainoff M, Maynard W, Robertson M, Anderson JH, 2012. Office Ergonomics. In Handbook of Human Factors and Ergonomics p.1561, Salvendy G (Ed.); Hoboken, New Jersey; John Wiley & Sons.
- Aaras A, Dainoff M, Ro O, et al. 2002. Can a more neutral position of the forearm when operating a computer mouse reduce the pain level for VDU operators?Int J Ind Ergon (30) 307–24.
- Gerr F, et al., 2002. A prospective study of computer users: I. Study design and incidence of musculoskeletal symptoms and disorders. Amer J of Indust Med (41) 221-235.
- Marcus M, et al, 2002. A prospective study of computer users: II. Postural risk factors for musculoskeletal symptoms and disorders. Amer J of Indust Med (41) 236-249.
- Cook C, Burgess-Limerick R. 2004. The effect of forearm support on musculoskeletal discomfort during call centre work. Applied Ergonomics (35) 337–342
- Gerr F, et.al., 2005. A randomized controlled trial of postural interventions for prevention of musculoskeletal symptoms among computer users. Occup Environ Med (62) 478-487
- Rempel D, Krause N, Goldberg R, et al. 2006. A randomized controlled trial evaluating the effects of two workstation interventions on upper body pain and incident musculoskeletal disorders among computer operators. Occup Environ Med (63) 300–306.
- Conlon C, Rempel D, Krause N. 2008. A randomized controlled trial evaluating an alternative mouse and forearm support on upper extremity body discomfort and musculoskeletal disorders among engineers. Occup Environ Med (65) 311–18.